Pharmacodynamic and Pharmacokinetic Interactions
Excerpt from Cafer's Mood Stabilizers and Antiepileptics
PHARMACODYNAMICS VS PHARMACOKINETICS
Drug-drug interactions fall into two main categories: pharmacokinetic and pharmacodynamic.
Pharmacodynamics is what a drug does to the body. Pharmacodynamic interactions are based on the drugs’ mechanisms of action and do not involve alteration in blood levels of either interacting drug.
Pharmacokinetics is what the body does to a drug. Kinetic derives from the Greek verb kinein, "to move”. In this case we’re talking movement into and out of the body, for instance absorbing the chemical from the gut and processing it for excretion in urine or feces. Pharmacokinetic (PK) interactions are generally manifested by alteration of blood levels of one of the interacting drugs.
For simplicity’s sake, let’s drop the pharmaco- prefix and refer to these concepts as kinetic interactions and dynamic interactions.
PHARMACODYNAMIC INTERACTIONS
Dynamic interactions are intuitive if you understand how the interacting drugs work. Although dynamic interactions are understandable without silly pictures, here are a couple anyhow.
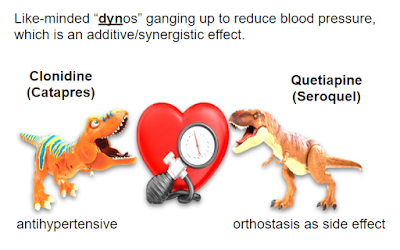
Dynamic interactions can be additive/synergistic, with enhanced effects brought about by combining medications with similar or complementary effects.
Other dynamic interactions are antagonistic, for instance combining a dopaminergic such as pramipexole (for restless legs) with an antidopaminergic like haloperidol (antipsychotic). Here’s another example:
PHARMACOKINETIC INTERACTIONS
Kinetics involves the rate at which a drug gets into or out of the body or brain.
Drug-drug Interactions involving absorption are generally straightforward. For instance, anticholinergics slow gut motility and delay gastrointestinal absorption of other medications.
Kinetic interactions involving rate of elimination from the body are challenging to learn and daunting to memorize. It is important to consider these interactions to avoid underdosing or overdosing certain medications. This book tackles these tricky elimination interactions by illustrating:
❖ Phase I metabolism involving the six most important cytochrome P450 (CYP450) enzymes
❖ Phase II metabolism involving UGT enzymes, as applicable to lamotrigine (Lamictal)
❖ Renal clearance of lithium (page 26)
A mysterious type of kinetic interaction involves drugs getting across the blood-brain barrier, as is necessary for a psychiatric medication to take effect. If such an interaction is occurring, the effect will not be detectable in serum drug levels. This will be discussed in the context of P-glycoprotein (page 9).
CYTOCHROME P450 ENZYMES
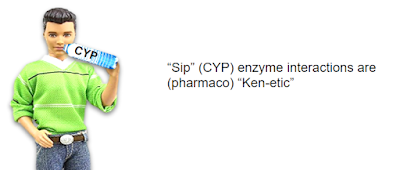
In the liver, kinetic interactions predominantly involve CYtochrome P450 enzymes, CYP enzymes for short, which can be pronounced “sip”. Instead of concerning yourself with the origin of P450 nomenclature, take a moment to contemplate this picture of Ken (kinetic) taking a “sip” (CYP).
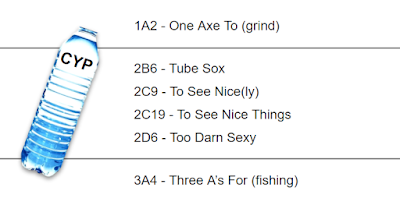
CYP enzymes, which reside primarily in the liver, make chemicals less lipid-soluble so they can be more easily excreted in urine or bile. Of over 50 CYP enzymes, six play a major role in the biotransformation of medications: 1A2, 2B6, 2C9, 2C19, 2D6 and 3A4. Our visual mnemonics will be built on the following phraseology:
The three most important CYPs are 1A2, 2D6 and 3A4. For psychiatrists, 2C19 can be important, while 2B6 and 2C9 are rarely significant.
Copyright 2020 CaferMed LLC




Comments
Post a Comment